No, not really. If your baby isn’t fussy, wakes up crying, or is constantly trying to pull their legs up to their tummy, they should be fine. Ideally, they should be burped after every meal, but don’t worry if you try and nothing comes out that time. Oftentimes they don’t have enough air to be uncomfortable during feedings or release it as they pass gas.
Why Your Baby Won't Burp and Techniques to Help
By: Dr. Maria Cerino - Updated May 15, 2024 - 11 Minute Read

From the moment our little ones home in our arms, a new chapter begins: feeding time. From choosing the right organic formula and breastfeeding to burping, tummy aches, and pooping schedules…it becomes a big stressor for most parents.
It's normal for newborns to have different nutritional needs than adults. Check out our article on how to burp your baby!
A Good Belch Can Calm Fussiness During And After Feedings
Everybody knows about belching. Most times, it comes to us in the most unexpected times, but the relief we feel is always unmatched. It’s no wonder babies find it extremely relieving; it’s what makes their stomachs settle after a feeding. It is only natural how their bodies release any extra air they might have ingested.
Burping them after feeding helps reduce fussiness, tummy pains, and other air-related issues. It also increases the possibility of them sleeping longer. However, not all babies burp the same way.
Some babies are natural at it and don’t need much more than a couple of pats on their back, while others struggle and require some extra attention. This is completely normal. In the rest of this article, we’ll describe each technique so you can be ready when you need it.

Why Won't My Baby Burp After Feeding?
When parents have their second child, they often compare their experiences with both babies. This can be a helpful way of framing their current situation, as it allows them to feel more confident in their parenting abilities. However, it is essential to remember that no two babies are the same, and each has their unique needs and preferences.
One area where babies can differ is in their feeding techniques and rates. Some babies may feed at a slower pace, while others may be more efficient. Sometimes, a baby may hold more air because of their feeding technique, which is okay. Some babies can quickly get rid of extra air by passing gas, while others may not swallow much air during feeding.
Furthermore, some babies can be extremely sleepy while feeding, and burping may not be their priority. They may fall asleep during or after feeding, making it challenging to burp them. However, this is not always a cause for concern, as some babies can easily tolerate this.
It is crucial to watch for warning signs that your baby is struggling to pass gas or burp.
● Hard, Bloated tummy to the touch
● Cries until their face turns red and pull their legs up to their tummy
● Their weight gain is slowed down because they stop feeding early
● Fusses during a feed and pulls away from the bottle

Can Your Baby Choke if Not Burped?
As a parent or caretaker, it's natural to worry about your baby's safety and well-being, especially when it comes to the risk of choking. One common concern is whether your baby may choke on their spit-up, particularly if they haven't burped. Fortunately, the likelihood of this happening is extremely low.
To further reduce the risk of choking, it's important to be mindful of how much you're feeding your baby and to keep their surroundings clean and free of any potential choking hazards. Doing so can help ensure that your baby's airways remain clear and they can breathe comfortably.
It's also worth noting that babies have a built-in reflex that allows them to swallow their spit-up, which helps keep their airways clear. If your baby does experience any discomfort or a sensation of food coming back up, they will typically wake up and cry, signaling that they need your help.
How Long Should I Try to Burp My Baby?
Burping a baby is a quick and easy process that takes only a few minutes. Some babies may need to be burped as soon as they finish feeding, while others may require them to be held upright for a while.
It is recommended to burp your baby after every 2-3 ounces of milk. You can also burp them when switching breasts to release any extra air and make room for more milk. Babies who swallow air tend to stop eating before they are full, which can slow down their growth and affect their nutrition.
Babies with severe reflux may need to stay upright for 30 minutes after eating, both day and night. If you choose to burp your baby on your lap, ensure their head is above their tummy for at least 15 minutes to prevent the milk from returning.

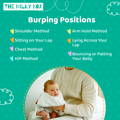
How to Burp a Baby: Effective Methods
The best way to burp your baby is to do what works best for them. It takes parents a few weeks to find a routine that works for them. Many factors will play a massive role in it: the type of bottle, the formula contents, the feeding position and their strength while sucking.
A few tips you should remember when burping your baby:
● Keep a soft cloth over your shoulder in case they spit up.
● Start patting from their diaper upwards until you reach their shoulders.
● Even if you don’t hear a loud burp after a few minutes of trying, the positioning and patting used for burping them is usually enough.
Change Baby's Position
Once families have the basics down, it’s time to talk positions. There is no “perfect” burping position, as babies change their preferences with time. We recommend you try all of them and stick to the one that feels most natural for you. Here are some of our preferred methods for your reference.
Shoulder Method
The shoulder method is the most frequently used. All you need to do is hold your baby upright on your chest. Their chest should be at your shoulder level. Make sure there’s no extra pressure on their throat. Support their body with one hand while you gently rub or pat their back to get the air out.
Sitting on Your Lap
For this method, you need to place them sitting on your lap, keeping their spine upright while supporting their chin and chest with one hand. Then, with your other hand, pat gently. This one is great for babies with reflux, as it helps them to keep their stomach upright for the first few minutes after feeding.
Chest Method
The chest method is good for keeping them asleep. It’s similar to the shoulder method, but this one requires you to hold your baby much higher. You will need to hold them up to your chest and support their buttocks with one of your hands. Some naturally put their legs up in a frog position, this is great news: it helps them pass gas. Then, just pat and rub their backs in a circular motion, and voilà!
Hip Method
The hip method works great when lying down, too. Place the baby’s tummy over your hip or belly while keeping their head above their body. You can then gently rub or pat their back between the shoulder blades.
Arm Hold Method
Sleeping babies love this position; it doesn’t disrupt their snoozing. You will need to lay your baby on your forearm face down, with their legs dangling on either side. Their head should fit the crook of your elbow, then pat up their back and rock them gently. This position is very relaxing for them!
Lying Across Your Lap
This requires them to be belly down across your lap. Make sure their head is a little raised in this position. Support their chin gently but do not put any pressure on the throat area, and use your free hand to rub or gently pat your baby’s back.
Bouncing or Patting Your Baby
It’s important to remember that the correct hand positioning for burping them is cupping your hand; this avoids using unnecessary strength but still transmits enough vibration to stimulate the airflow.
Ideally, you need to work your way up their back. Some parents start at their baby’s bottom, and they swear by it. It doesn’t hurt to try it out if you’re struggling with getting your baby to burp. Rubbing their backs works wonders, too, so you might try incorporating some rubbing in between pats.
Many parents suggest bouncing them when burping them while sitting on your lap. This is okay as long as it’s a very gentle movement. You can softly bounce your leg up and down, but we don’t recommend using this technique if your baby burps just fine with some patting and rubbing.
Babies, particularly very small ones, have very fragile bones and nerves in their heads and necks, and vigorous bouncing could hurt their spinal tract or brain forever, so we recommend all bouncing to be extremely gentle.
What to Do if Your Baby Doesn't Want to Burp?
If you have tried a few different methods, you might want to try setting them down for a little and trying again, but if your baby isn’t showing any discomfort, they might not have enough air in their digestive system to form a bubble. It’s not necessarily a bad sign; some babies are also naturally more prone to pass gas instead of burping.
In 2014, researchers found in a very interesting study, that there was no decreased risk of suffering colics in babies who are regularly burped. While it is a rite of passage, and we still recommend you to attempt it after every feeding, your baby isn’t at any increased risk of pain if they aren’t huge on burping.
Lastly, if your baby tends to be on the gassier side, there are some great ways to help them out before and during feedings.
Here are some tips for preventing trapped air bubbles whether you are breastfeeding or bottle-feeding.
For Bottle-Fed Babies:
1. Position the bottle horizontally to feed your baby. When fed while lying down with an upright bottle, babies tend to drink quickly, risking overfeeding.
2. Monitor the milk flow closely. Rapid milk flow can lead to babies taking in excess air. Consider switching to a wider-mouthed nipple with a slower flow to prevent this issue.
3. Ensure your baby's head is positioned higher than their tummy during feeding. Use a cushion or nursing pillow to find a comfortable position.
4. Encourage breaks during feeding sessions. Avoid letting your baby drink too quickly. Pause every few ounces and employ 'paced' bottle feeding techniques.
5. If your baby is frequently experiencing gas or difficulty in passing gas, it might be helpful to consider using a formula designed to ease their digestion. It is recommended to choose a formula that uses clean and organic ingredients with baby probiotics that can help balance their gut with healthy bacteria. This may help alleviate your baby's discomfort and improve their overall digestive health.
For Breastfeeding Babies:
1. Check their latching position: Ensure minimal or no areola is visible. Your baby's chin should contact your breast, their lips should be flared outward like a fish, and their ears should gently move as they suckle.
2. Check your breastfeeding position: It’s healthier for babies to nurse when their head is higher than their body. Trying out a few positions might do the trick for them.
European Baby Formulas for Gas
European Baby Formulas are specifically designed to emulate the nutritional profile of breast milk, including the right balance of proteins, fats, carbohydrates, vitamins, and minerals.
They are also formulated to be easily digestible, which is crucial for an infant's delicate digestive system.

In Conclusion…
Preventing gas in babies is extremely helpful for their comfort, but remember that not all babies breathe in the same amount of air during feedings. If your burping technique is correct, they’re latching on correctly while breastfeeding or taking their bottle the right way, and they don’t show any discomfort, you’ve got nothing to worry about.
However, if your baby experiences constant discomfort while feeding, is constantly bloated, or suffers from other symptoms, such as blood in their poop, it might be time to consult your pediatrician or other qualified practitioner. Some babies have food allergies and might require a specialized formula to get their nutrition right.
As always, The Milky Box is here for all your baby's nutritional needs, from organic to vegan formulas. We’re only a few clicks away.
Frequently Asked Questions
Is it bad if my baby goes to sleep without burping?
At what age should I stop burping my baby?
Babies stop needing to be burped once their digestive system has matured with their natural growth. For most babies, you can stop burping them at around 4-6 months. After that, particularly when solids start being introduced, you will notice them burping on their own accord.
Should I use an OTC drop to help my baby burp?
We strongly discourage using OTC products or gripe water without consulting your doctor first, as these could harm your baby’s GI tract. If fussiness after feeding persists, it might be better to get them checked out with their pediatrician, as they could suffer from a food allergy or enzyme deficiency that could make digestion uncomfortable.
Can I stop burping my baby if they already burped once?
You should be okay if they’ve gone back to sleep and everything seems fine. When parents stop feeding every few seconds to keep burping the baby, it disrupts their feeding routine. This frustrates the baby and can also lead to them abandoning the feeding session earlier than they need.
Do the foods that I eat contribute to my baby’s gassiness?
Yes and no. This question is divisive, and even health authorities don’t have a definite answer. The most common culprits banned by many parents are cabbage, beans, leafy greens, and garlic. The truth is that there is no evidence backing up this fact, but many moms swear by it.
We recommend you test it out, if your baby’s feeding normally goes after eating them, you should be good. Babies with food allergies can greatly benefit from specialized formulas suited to their individual needs.
Disclaimer:
Please be aware that this information is based on general trends in babies, and it is not medical advice. Your doctor should be your first source of information and advice when considering any changes to your child’s formula and when choosing your child’s formula. Always consult your pediatrician before making any decisions about your child’s diet or if you notice any changes in your child.
Breastfeeding is the best nutrition for your baby because breast milk provides your child with all the essential nutrients they need for growth and development. Please consult your pediatrician if your child requires supplemental feeding.

Dr. Maria Cerino is a medical doctor and a researcher from Mexico, her works being published in prestigious journals like the American Journal of Human Biology among others. As a medical writer, Dr. Cerino focuses on infant nutrition and healthy neurological development in infants and children. In her free time, she enjoys going on walks, watching indie films, and cooking at home.
Read Next:
Reviewed by Dr. Eric Wood, ND, MA

Dr. Wood is a licensed naturopathic doctor, with a doctorate degree from the Canadian College of Naturopathic Medicine in Toronto, Canada. He received his post-graduation certification in Mind Body Medicine at Harvard University.
With 15 years of experience, Dr. Wood is an Associate Professor of Holistic Nutrition at the American College of Health Sciences in Portland, Oregon. Dr. Wood is an educator, clinician, author, media figure, consultant, and owns his own holistic (naturopathic) medical practice in Ft. Lauderdale, Florida. Dr. Wood is currently researching and drafting books on cancer and pediatrics.
Outside of the medical profession, Dr. Wood loves singing with the Miami Lyric Opera and is an avid musician in South Florida. He also loves spending time with his wife and kids.

